Fasting tips for diabetes control require careful planning to avoid hypoglycemia, hyperglycemia, and other complications. Research indicates that structured fasting protocols, combined with medical supervision, can improve insulin sensitivity and metabolic health. This guide outlines evidence-based strategies for individuals with type 1, type 2, or gestational diabetes considering intermittent or prolonged fasting.
Understanding Diabetes and Fasting
How Fasting Affects Blood Sugar
Fasting alters glucose regulation by depleting glycogen stores and shifting the body to fat metabolism. For diabetics, this process can lead to unpredictable blood sugar fluctuations:
| Fasting Stage | Impact on Blood Sugar |
|---|---|
| 0–4 hours | Stable (glycogen usage) |
| 4–12 hours | Gradual decline |
| 12–24 hours | Ketosis begins |
| 24+ hours | Risk of hypoglycemia |
Risks and Benefits
- Benefits: Improved insulin sensitivity, weight loss, reduced inflammation.
- Risks: Severe hypoglycemia, dehydration, ketoacidosis (type 1 diabetes).
Consult healthcare providers before starting any fasting regimen. For meal planning insights, explore the NIME diet.
7 Fasting Tips for Diabetes Control
1. Choose a Fasting Method Aligned With Health Status
- Intermittent Fasting (12–16 hours): Suitable for type 2 diabetics with stable HbA1c levels.
- Time-Restricted Eating: Limit eating windows to 8–10 hours daily.
- Avoid prolonged fasts (>24 hours) without medical oversight.
2. Monitor Blood Sugar Frequently
Check glucose levels:
- Before fasting
- Every 2–4 hours during fasting
- After breaking the fast
Use continuous glucose monitors (CGMs) for real-time data.
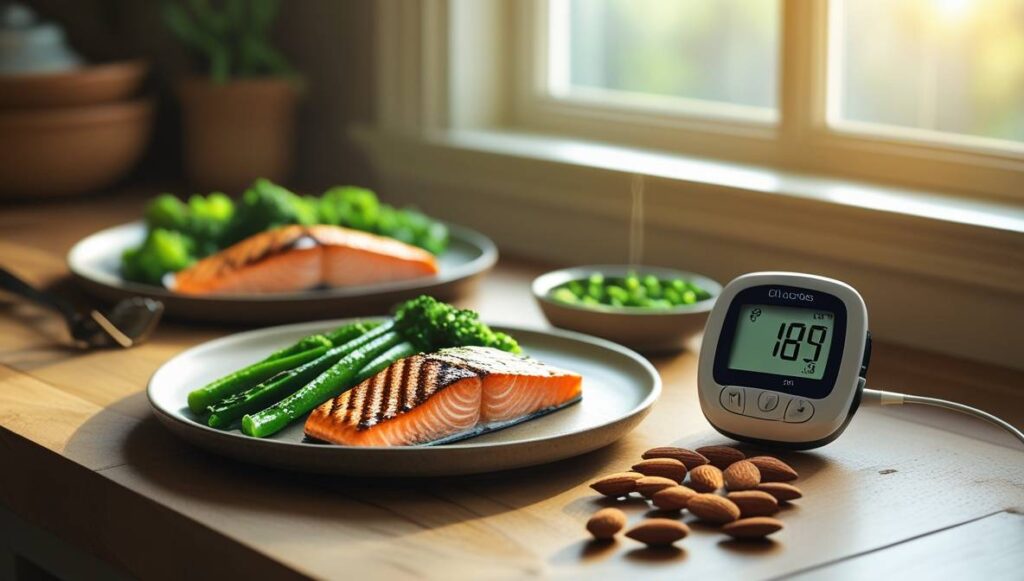
3. Prioritize Nutrient-Dense Meals
Pre-fasting meals should balance macronutrients:
| Component | Recommended Intake |
|---|---|
| Protein | 20–30% of calories |
| Healthy fats | 30–40% of calories |
| Fiber | 25–35 grams daily |
For recipes, see cottage cheese recipes.
4. Stay Hydrated
Dehydration exacerbates blood sugar spikes. Consume:
- Water: 2–3 liters daily
- Electrolytes: Sodium, potassium, magnesium
Avoid sugary drinks and excessive caffeine.
5. Adjust Medications
Work with healthcare providers to modify insulin or oral medications. Sulfonylureas and insulin doses often require reduction during fasting.
6. Break Fasts Gradually
- Start with small portions of protein and fiber.
- Avoid high-carb meals to prevent rebound hyperglycemia.
7. Recognize Warning Signs
Stop fasting if experiencing:
- Dizziness
- Confusion
- Blood sugar <70 mg/dL or >300 mg/dL
For emergency strategies, read managing joint pain.
Meal Planning During Fasting Windows
Sample Pre-Fast Meal
- Grilled chicken (6 oz)
- Steamed broccoli (1 cup)
- Quinoa (½ cup)
- Olive oil (1 tbsp)
Sample Post-Fast Meal
- Greek yogurt (1 cup) with almonds (10–12)
- Spinach salad with avocado
- Salmon (4 oz)
For portion guidelines, refer to how many almonds kids should eat.
Special Considerations
Type 1 Diabetes
- Higher risk of ketoacidosis. Monitor ketone levels using urine strips.
- Avoid fasting during illness or unstable glucose periods.
Gestational Diabetes
- Short fasting windows (8–10 hours) only under obstetrician guidance.
- Prioritize protein intake to support fetal development.
Elderly Patients
- Higher hypoglycemia risk. Opt for 12-hour fasts maximum.
- Ensure adequate hydration and electrolyte balance.
Learn about early-onset menopause and its metabolic implications.
FAQs
Can fasting reverse type 2 diabetes?
Fasting may improve insulin sensitivity but is not a cure. Pair with lifestyle changes for sustained results.
Is Ramadan fasting safe for diabetics?
Yes, with adjusted medication, frequent monitoring, and balanced suhoor/iftar meals.
Does fasting reduce insulin resistance?
Studies show intermittent fasting lowers HbA1c by 1–2% in prediabetic individuals.
For multilingual health resources, visit Apple Intelligence expands multilingual support.